Interview with worldwide experts on antibiotic resistance outlines recommendations for policymakers
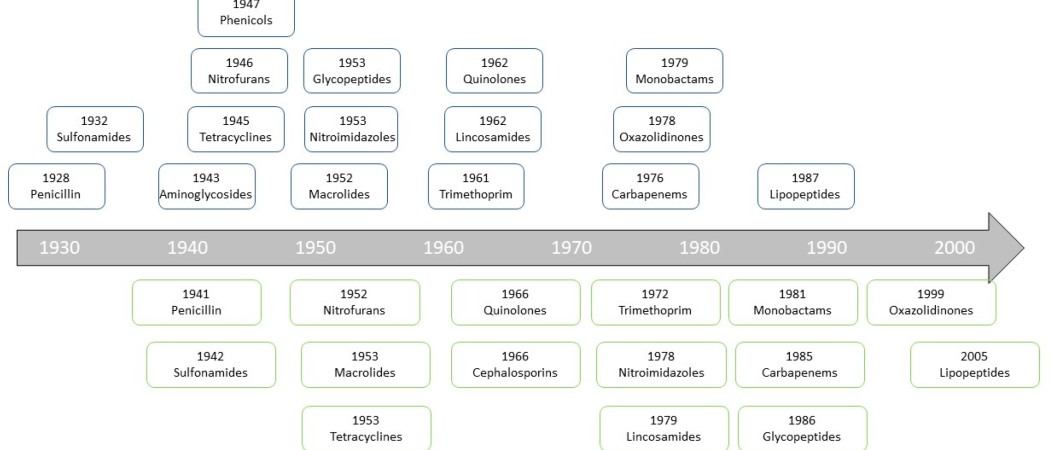
Timeline of antibiotic discovery and emergence of resistance. Source: article.
Leading experts from the European Academy of Microbiology discuss the issue of antimicrobial resistance. Key actions include promotion of dialogue, public outreach and education, curation of public databases, and creating the right incentives for drug companies.
“For every complex problem,” according to journalist and essayist Henry Louis Mencken “there is an answer that is clear, simple, and wrong.”
In the case of antibiotic resistance, the opposite seems the case. Resistance to antibiotics is a simple phenomenon, for which a complex solution is needed. But what is the right answer to address this problem?
Exposure of bacteria to antibiotics correlates with the emergence, extent and prevalence of antibiotic-resistant strains, both in the environment and in the clinic, and resistance to a new drug usually emerges within a few years after it is introduced on the market.
To revert this problem, a whole series of actions are needed, as the speed at which new antibiotics are discovered and released into the market is much slower than that at which resistance emerges.
These actions include reducing the use of antibiotic, but the reality of facts is more complex, and ongoing research, continuous monitoring and improved therapies are required. This and further societal and economic factors make the formulation of relevant policies an extremely difficult task.
Recently, the European Academy of Microbiology (EAM) organised a workshop with worldwide experts on antimicrobial resistance, the results of which were published in “Antibiotic resistance: turning evolutionary principles into clinical reality” on FEMS Microbiology Reviews.1
One key outcome is that we have not yet reached the tipping point, as currently available antibiotics, if used wisely and more efficiently than what is the case now, will retain the potential to successfully eradicate bacterial pathogens. Favouring this is the deposition of research and clinical data, including genomic and molecular information, in publicly accessible databases.
We spoke with the authors to gain more insights on their expert opinion, in particular regarding broader challenges that society faces, and recommendations on the topic emerging from their position paper.
If you are to rank (i) release of new drugs, (ii) development of new approaches, or (iii) less use of existing antibiotics, which would be a short-, mid- or long-term priority?
We should simultaneously fight on all three fronts now! Of course, release of new drugs will take more time than developing antibiotic stewardship. While reducing the use of existing antibiotics per se is important, the right use of them is key. For this, we need to better educate the broader public, farmers, veterinarians, medical doctors and nurses. Important progresses have already been made in this field. The role of pharmacists that refuse selling antibiotics without prescription should be acknowledged more.
For low- and medium-income countries, availability of high-quality products with appropriate drug concentrations is necessary.
What would be the incentive for industry to remain on the frontline of antimicrobial research?
Antibiotics for common, extensive use in non-life-threatening infections should be cheap and non-toxic. Yet we should accept that antibiotics against infection by multi-resistant organisms in high-risk hosts can be much more expensive, as the number of treated cases is low. In some last-resort cases, a higher toxicity should be considered, as this is the case for anti-cancer drugs.
The possibility to revive drug projects that did not make it to the market represents an opportunity as well. Many pilot antibiotics have been abandoned since they lack a broad spectrum of activity. These drugs can be quite valuable for treating specific infections, with lower side effects for the human microbiome. Research on combination therapies has been discontinued in previous decades, but these are more effective in preventing resistance.
The positive image that drug companies might gain in the public eyes and in those of professionals could represent a powerful incentive too.
A recent article underlined the need for microbiology literacy in society.2 In the case of antibiotic resistance, would educating or campaigning be more important?
Both are, and they should be done synergistically! Today, in the age of the microbiome, people are becoming more aware that inappropriate use of antibiotics is hurting themselves first, both by generating resistant bacteria that can persist in their bodies for years and by eliminating beneficial symbionts. This provides the opportunity to have a larger impact, and make the public conscious that the problem has an ecological dimension, as antibiotic resistance can be considered an environmental pollutant.
Defining the best communication strategy should involve a dialog with experts in the humanities and social sciences too. Microbiologists should work with psychologists, sociologists, and communication experts to deliver the message effectively.
What would be two single actions that people can adopt in every-day life to contribute against the rise of antibiotic resistance?
People should vaccinate themselves and their children according to national recommendations, which should reduce the burden of preventable infectious disease, and with it the prescription and consumption of antibiotics.
Unsolicited antibiotic prescriptions (for example following a viral infection, like a common cold) and self-medication with antibiotics from previous treatments must be avoided.
What would be clear, actionable recommendations for policymakers emerging from your paper?
- Favour education of the broad public as well as training of professionals on antibiotics and their proper use
- Reinforce global surveillance and hygiene recommendations in health care institutes
- Promote a constant and critical debate among experts and practitioners as knowledge on antibiotic resistance evolves rapidly but it rarely influences clinical practice
- Promote the collection of clinical data in unified, public databases
- Provide right incentives for drug companies, including the continuous support of public-private associations such as the EU’ Innovative Medicines Initiative (IMI-ENABLE)
- Ban antibiotics as animal food additive in countries where they are still in use
- Consider global equality as a form of ‘selfish equality’ by increasing the wealth and dignity of people around the world (for instance, with a focus in sanitation in areas where poor conditions and unregulated antibiotic use favour spread of resistance)
For more information, please contact [email protected]
1 Antibiotic resistance: turning evolutionary principles into clinical reality. Dan I Andersson, Nathalie Q Balaban, Fernando Baquero, Patrice Courvalin, Philippe Glaser, Uri Gophna, Roy Kishony, Søren Molin, Tone Tønjum. FEMS Microbiology Reviews, 25 January 2020 (doi.org/10.1093/femsre/fuaa001). https://doi.org/10.1093/femsre/fuaa001
2 The urgent need for microbiology literacy in society. Kenneth Timmis, Ricardo Cavicchioli, José Luis Garcia, et al. Environmental Microbiology, 25 March 2019 (doi.org/10.1111/1462-2920.14611). https://sfamjournals.onlinelibrary.wiley.com/doi/full/10.1111/1462-2920.14611



 A unique international forum for public research organisations and companies to connect their external engagement with strategic interests around their R&D system.
A unique international forum for public research organisations and companies to connect their external engagement with strategic interests around their R&D system.