The past decade has seen the rise of a new movement in healthcare policy: patient-centred thinking that tries to include in the policy mix what patients themselves think of their treatments, and the outcomes. The idea is that taking this into account will lead to more effective treatments, lower costs and higher quality of life – and so far, the experience in those clinics and countries that have adopted the practice has been encouraging. Leaders in this field include the Swedish, Dutch, British and parts of the US health systems; and individual clinics in some countries have reported spectacular results. The European Commission has recently made adoption of this thinking a priority in health policy.
Here, Science|Business Healthy Measures provides a quick guide to some of the best literature on the topic.
Enhancing value in European health systems: The role of outcomes measurement (FIPRA)
 A 2016 policy paper that showcases the importance of measuring outcomes for greater transparency in and oversight of the performance of European healthcare systems. It summarises initiatives in different EU member-states, highlighting how different clinics and health authorities have improved their results by measuring and tracking patient-reported outcomes. It argues that such measures should be included in assessments of health system performance. A multi-stakeholder initiative endorsed by 12 patient, academic and industry groups, and organised by FIPRA.
A 2016 policy paper that showcases the importance of measuring outcomes for greater transparency in and oversight of the performance of European healthcare systems. It summarises initiatives in different EU member-states, highlighting how different clinics and health authorities have improved their results by measuring and tracking patient-reported outcomes. It argues that such measures should be included in assessments of health system performance. A multi-stakeholder initiative endorsed by 12 patient, academic and industry groups, and organised by FIPRA.
From the report:
“Outcomes measurement for prostate cancer began at the Martini Klinik (in Germany) in 1994, with data initially recorded using an Excel table, but now via an electronic database. A range different outcomes data is collected: clinical (e.g. positive surgical margin – used after surgery to determine whether further treatment/surgery may be required), mortality, administrative (e.g. surgery and radiotherapy), and patient-reported (e.g. urinary function, and quality of life). Every six months, risk adjusted data for each surgeon is shared with the full team. A three-hour quality review meeting is held to analyse the results, and a biostatistician is tasked with analysing the data to help frame the discussion. As a result of these meetings, surgeons with the best results may observe surgeons with below average results, and those with higher complication rates may be assisted in surgery by more experienced surgeons. The outcomes produced by Martini Klinik are impressive – performing significantly better than the national (German) average on a number of measures. For example, the proportion of patients reporting:
“Any incontinence:
- Martini Klinik: 6.5%
- National average: 43.3%
Severe urinary incontinence:
- Martini Klinik: 0.4%
- National average: 4.5%
Severe erectile dysfunction:
- Martini Klinik: 34.7%
- National average: 75.5%
“Martini Klinik’s five-year survival rates for prostate cancer are also above the national average.”
The strategy that will fix health care (Harvard Business Review)
A 2013 Harvard Business Review paper by two leading advocates of ‘value-based’ healthcare reforms, Michael E. Porter of Harvard University and Thomas H. Lee of Press Ganey Associates. A good summary of the research into and arguments for using patient-centred measures to make health systems work better and more efficiently across the world.
From the report:
“In health care, the days of business as usual are over. Around the world, every health care system is struggling with rising costs and uneven quality despite the hard work of well-intentioned, well-trained clinicians. Health care leaders and policy makers have tried countless incremental fixes—attacking fraud, reducing errors, enforcing practice guidelines, making patients better “consumers,” implementing electronic medical records—but none have had much impact.
It’s time for a fundamentally new strategy.
At its core is maximizing value for patients: that is, achieving the best outcomes at the lowest cost. We must move away from a supply-driven health care system organized around what physicians do and toward a patient-centred system organized around what patients need. We must shift the focus from the volume and profitability of services provided—physician visits, hospitalizations, procedures, and tests—to the patient outcomes achieved. And we must replace today’s fragmented system, in which every local provider offers a full range of services, with a system in which services for particular medical conditions are concentrated in health-delivery organizations and in the right locations to deliver high-value care.”
Doctor spending enough time with patient in consultation, 2013 (or nearest year).
Health at a Glance 2015 (OECD)
As part of its regular review of health systems in the developed countries, the Organisation for Economic Cooperation and Development has been incorporating more statistics on what patients think of their treatments. This site includes a selection of results, and recommendations.
From the report:
“A growing number of countries are using patient-reported data to drive quality improvements in health systems. Patient experience data are reported in periodic national health system reports or on public websites, showing differences across providers, regions and over time. Korea, Norway, Sweden and the United Kingdom use patient experience measures in payment mechanisms or for fund allocations to promote quality improvement and patient-centred care, and Australia, Canada, the Czech Republic, Denmark and France use them to inform health care regulators for inspection, regulation and/or accreditation. Patient-reported measures are also used in some Canadian jurisdictions, Denmark, France and the Netherlands to provide specific feedback for providers' quality improvement. In England, PROMs and patients' feedback about their experience are used to inform patient choice and to incentivise service improvement. For example, PROMs data for patients undergoing some procedures such as hip and knee replacement are used for benchmarking hospitals. The use of PROMs can also enable the potential shift from a volume-based to a value-based model of health system resource management (Canadian Institute for Health Information, 2015).”
Read the report Download statistics
Getting the most out of PROMs: Putting health outcomes at the heart of NHS decision-making (King’s Fund)
 A very comprehensive 2011 report that contains a basic introduction to PROMs and their potential to improve healthcare services, as well as recommendations for methods of data collection and interpretation and understanding outcomes. Included is an explanation of what duties particular healthcare organizations, hospitals and their clinicians as well as government authorities would have to take on in order to develop PROM-based healthcare.
A very comprehensive 2011 report that contains a basic introduction to PROMs and their potential to improve healthcare services, as well as recommendations for methods of data collection and interpretation and understanding outcomes. Included is an explanation of what duties particular healthcare organizations, hospitals and their clinicians as well as government authorities would have to take on in order to develop PROM-based healthcare.
From the report:
“There has been a marked shift internationally in thinking about what health is and how it is measured. Traditional clinical ways of measuring health and the effects of treatment are increasingly accompanied by, or indeed replaced by, PROMs. In broad terms, PROMs comprise a series of structured questions that ask patients about their health from their point of view…
“This shift in focus is most evident in the appraisal of new health care technologies, where products and practices are subject to rigorous evaluation. The United States’ Food and Drug Administration (FDA), which has recently recommended the inclusion of patient reported outcomes (PRO) in US clinical trials (Food and Drug Administration 2006), notes: ‘the use of PRO instruments is part of a general movement toward the idea that the patient, properly queried, is the best source of information about how he or she feels’ (Bren 2006).
“In parts of the NHS, most notably in the appraisal of new health technologies by the National Institute for Health and Clinical Excellence (NICE) (National Institute for Health and Clinical Excellence 2008a), the use of PRO data is already commonplace, and, indeed, is a required part of the evidence used in the appraisal of, and decision-making about, health technologies. Over the course of several decades, clinical, health services and social sciences researchers have produced literally thousands of validated instruments that facilitate the consistent, reliable measurement of patient-reported health. Patients’ perspectives on their health outcomes can now be measured in most clinical areas.”
Building national outcomes registries in the Netherlands: The Dutch Institute for Clinical Auditing (ICHOM)
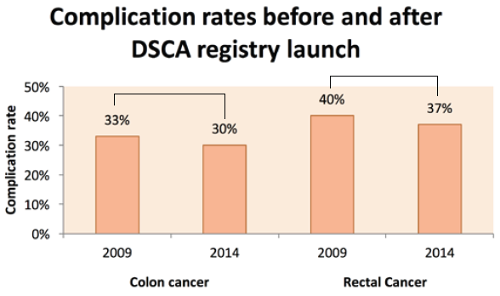 This 2016 case study describes the Dutch experience with outcomes measurement, since it launched a set of data registries to track outcomes in various disease categories. Its data on reductions in colorectal cancer complications are particularly striking, and include the business case for payer investment in outcomes registries, benefits to stakeholders and positive early results in patient outcomes improvement and cost reduction. Report by the International Consortium for Health Outcomes Measurement, based on Dutch data.
This 2016 case study describes the Dutch experience with outcomes measurement, since it launched a set of data registries to track outcomes in various disease categories. Its data on reductions in colorectal cancer complications are particularly striking, and include the business case for payer investment in outcomes registries, benefits to stakeholders and positive early results in patient outcomes improvement and cost reduction. Report by the International Consortium for Health Outcomes Measurement, based on Dutch data.
From the report:
"Since the start of the DSCA registry, complication rates for colorectal surgery patients have reduced and are expected to continue to do so as quality improvement project loops are completed. Since complications represent a significant cost burden, this fall in complication rates represents a significant reduction in costs. For example, DICA reported a reduction in severe complication rates after implementation of the DSCA audit from 25% to 20% between 2010 and 2012. As described, in DICA’s 2015 study by J.A. Govaert and colleagues, if a hospital were to perform 100 colorectal cancer procedures per year and had an average severe complication rate reduction of 10% between 2010 and 2012, this would lead to a saving of €120,000 (one major complication is associated with a €16,059 increase in cost). Subtracting the cost of participation in the DSCA (€13,350 per year), the overall profit for a single hospital would still be over €80,000. This provides a strong business case for outcomes measurement implementation.”
Patient reported outcome measures in practice (BMJ)
 A short review article advocating the wider use of patient-reported outcome measures, including a useful summary of the Swedish experience with registering data from rheumatology patients to reduce complications. Authors led by a Dartmouth College professor, published in the British Medical Journal in 2015.
A short review article advocating the wider use of patient-reported outcome measures, including a useful summary of the Swedish experience with registering data from rheumatology patients to reduce complications. Authors led by a Dartmouth College professor, published in the British Medical Journal in 2015.
From the report:
“Evidence shows that the systematic use of information from PROMs leads to better communication and decision making between doctors and patients and improves patient satisfaction with care. There is also evidence that patients report better outcomes—for example, improvement in depression. However, research on attempts to embed measurement of patient reported outcomes into routine practice has revealed many technical, social, cultural, legal, and logistical barriers to successful adoption. Clinicians are often reluctant to use PROMs routinely because they fear it will add to their workload rather than make them more efficient and effective. Furthermore, many clinicians who do spend time talking to patients contend that they already understand their patients’ problems and do not need additional information from them. Patients generally welcome systems that routinely use PROMs. However, they say that patient reporting systems must be used well and not misdirect the focus of the clinical encounter, burden patients, or focus only on factors that have value to clinicians.”
Strategies for overcoming barriers to the implementation of patient-reported outcome measurements (NIH)
 A 2014 paper for the US National Institutes of Health analysing the barriers to the adoption of patient-reported outcome measures, and offering proposals for patients and clinicians to overcome them.
A 2014 paper for the US National Institutes of Health analysing the barriers to the adoption of patient-reported outcome measures, and offering proposals for patients and clinicians to overcome them.
From the report:
"In most published examples of routine PRO collection, clinician barriers to using PROs include: a) the concern that the PRO instrument will uncover issues that clinicians feel incapable of handling, or that they will become liable for if inadequately addressed; b) that the collection and utilization of PROs will disturb work flows and decrease efficiency; c) that the benefit to patient care will be only theoretical and unsubstantiated; and d) that managing responses will be just another responsibility for already overburdened clinicians. On a more basic level, some clinicians may be hesitant to incorporate PROs into routine care because they are unsure how to make use of the data and might require support (personnel or information technology) to help navigate the information provided by the patient. Currently, one of the biggest barriers to PRO implementation is reluctance to change.”
The patients’ charter on patient empowerment (EPF)
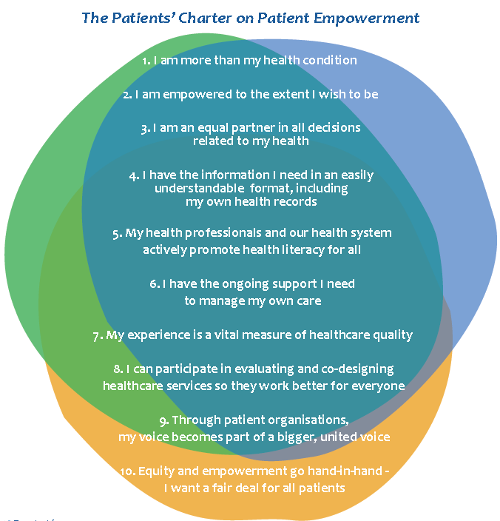 This poster summarises fundamental principles of patient empowerment and patient-centered healthcare from the patients’ perspective. It lays out principles that matter to patients, to improve healthcare policy to promote the message of patient empowerment. It was developed as part of a campaign by the European Patients’ Forum and the Robert Bosch Stiftung, with the support of Amgen, GSK and MSD.
This poster summarises fundamental principles of patient empowerment and patient-centered healthcare from the patients’ perspective. It lays out principles that matter to patients, to improve healthcare policy to promote the message of patient empowerment. It was developed as part of a campaign by the European Patients’ Forum and the Robert Bosch Stiftung, with the support of Amgen, GSK and MSD.
From the report:
“I am an equal partner in all decisions related to my health. All health-related decisions, whether long-term care planning for complex needs or one-off treatment/prevention decisions, should be the result of a shared decision-making process between the patient and the healthcare team. Patients manage their chronic condition themselves most of the time. Patients and professionals need to build a relationship based on mutual respect, share information and engage as equal partners in dialogue about treatment preferences, priorities and values.”
Patient-reported outcomes (Cochrane)
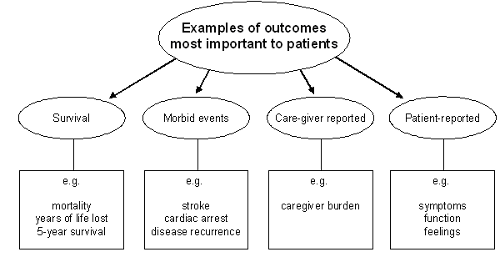 This document contains background on patient-reported outcomes, different classifications, taxonomy and methods of collection, as well as examples of patient-centred health methods that have been implemented so far by different hospitals. It is a guide for researchers and doctors, from the Cochrane group, which compiles international expertise into guidelines for practitioners. This particular section is from the Cochrane Handbook for Systematic Reviews of Interventions.
This document contains background on patient-reported outcomes, different classifications, taxonomy and methods of collection, as well as examples of patient-centred health methods that have been implemented so far by different hospitals. It is a guide for researchers and doctors, from the Cochrane group, which compiles international expertise into guidelines for practitioners. This particular section is from the Cochrane Handbook for Systematic Reviews of Interventions.
From the report:
“Elicitation of concepts and items for a PRO questionnaire should come from qualitative research with patients, family members, clinical experts, and the literature… For example, authors of a Cochrane review of cognitive behavioural therapy (CBT) for tinnitus included quality of life as an outcome (Martinez-Devesa 2007). Quality of life was assessed in four trials using the Tinnitus Handicap Questionnaire, in one trial the Tinnitus Questionnaire, and in one trial the Tinnitus Reaction Questionnaire. The original sources are cited in the review. Citations to articles on the psychometric properties are also available in MEDLINE for all three instruments and could easily be identified with a search using the Google search engine. Information on the items and the concepts measured are contained in these articles, and review authors were able to compare the content of the instruments.
“Another issue to consider in understanding what is being measured is how the PRO instruments are weighted. Many specific instruments weight items equally when producing an overall score. Utility instruments designed primarily for economic analysis put great stress on item weighting, attempting to present HRQOL as a continuum anchored between death and full health. Readers interested in the issues we have laid out in the previous paragraph can look to an old, but still useful summary (Guyatt 1993).”

 A unique international forum for public research organisations and companies to connect their external engagement with strategic interests around their R&D system.
A unique international forum for public research organisations and companies to connect their external engagement with strategic interests around their R&D system.